QoL and Patient-Reported Outcome and Supportive Care
Poster Session 3
P-451: Association between Dexamethasone Exposure and Visually Significant Cataracts in Myeloma
Friday, September 29, 2023
1:15 PM - 2:15 PM EEST

Rahul Banerjee, MD
Assistant Professor, Clinical Research Division
Fred Hutchinson Cancer Center
Seattle, Washington, United States
Introduction: Ocular comorbidities such as cataracts, which may lead to blurry vision and QOL impairments, are more common in relapsed multiple myeloma (MM) than in new diagnoses (Ailawadhi 2022). Pre-belantamab ophthalmological analyses from DREAMM-2 [3+ prior lines of therapy (LoT), over half aged ≥65] showed that 60% of pts with relapsed/refractory MM had cataracts at baseline (Popat 2022). In contrast, only 34% of US adults aged ≥65 have cataracts (Wittenborn 2023). We hypothesized that dexamethasone (dex) dose intensity and duration would predict both cataract occurrence as well as visual significance (pt-reported interference with QOL).
Methods: This was a secondary analysis of pt-reported treatment data collected from users of the HealthTree Cure Hub for Multiple Myeloma database. Pts who recalled developing cataracts with any LoT were asked to rate their cataract-related symptoms on a 1-5 Likert scale. Dex exposure was assessed by calculating the total duration and dosage across all LoTs until cataracts were first reported; cycles were assumed to be 28 days long regardless of regimen. Time-to-cataract survival analyses were conducted to assess the risk of cataracts. Ordinal logistic regression and correlation analyses were performed to evaluate the association between dex exposure and cataract severity.
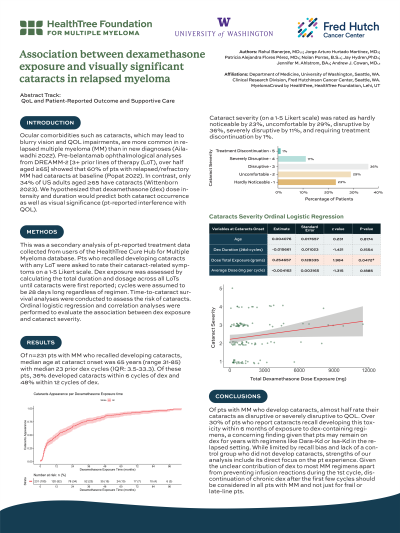
Results: Of n=231 pts with MM who recalled developing cataracts, median age at cataract onset was 65 years (range 31-85) with median 23 prior dex cycles (IQR: 3.5-33.3). Of these pts, 36% developed cataracts within 6 cycles of dex and 48% within 12 cycles of dex. Cataract severity (on a 1-5 Likert scale) was rated as hardly noticeable by 23%, uncomfortable by 29%, disruptive by 36%, severely disruptive by 11%, and requiring treatment discontinuation by 1%. Ordinal regression analyses of 97/231 pts with detailed dex dosing data available (from concurrent chart review) showed a significant association between total dex exposure and cataract severity (coefficient estimate [ce] 0.255, p< 0.05), which was confirmed by correlation analysis (r=0.143). However, age at cataract onset (ce 0.004, p=0.81) and dex dose per cycle (ce -0.004, p=0.19) did not show a significant relationship with cataract severity.
Conclusions: Of pts with MM who develop cataracts, almost half rate their cataracts as disruptive or severely disruptive to QOL. Over 30% of pts who report cataracts recall developing this toxicity within 6 months of exposure to dex-containing regimens, a concerning finding given that pts may remain on dex for years with regimens like Dara-Kd or Isa-Kd in the relapsed setting. While limited by recall bias and lack of a control group who did not develop cataracts, strengths of our analysis include its direct focus on the pt experience. Given the unclear contribution of dex to most MM regimens apart from preventing infusion reactions during the 1st cycle, discontinuation of chronic dex after the first few cycles should be considered in all pts with MM and not just for frail or late-line pts.
Methods: This was a secondary analysis of pt-reported treatment data collected from users of the HealthTree Cure Hub for Multiple Myeloma database. Pts who recalled developing cataracts with any LoT were asked to rate their cataract-related symptoms on a 1-5 Likert scale. Dex exposure was assessed by calculating the total duration and dosage across all LoTs until cataracts were first reported; cycles were assumed to be 28 days long regardless of regimen. Time-to-cataract survival analyses were conducted to assess the risk of cataracts. Ordinal logistic regression and correlation analyses were performed to evaluate the association between dex exposure and cataract severity.
Results: Of n=231 pts with MM who recalled developing cataracts, median age at cataract onset was 65 years (range 31-85) with median 23 prior dex cycles (IQR: 3.5-33.3). Of these pts, 36% developed cataracts within 6 cycles of dex and 48% within 12 cycles of dex. Cataract severity (on a 1-5 Likert scale) was rated as hardly noticeable by 23%, uncomfortable by 29%, disruptive by 36%, severely disruptive by 11%, and requiring treatment discontinuation by 1%. Ordinal regression analyses of 97/231 pts with detailed dex dosing data available (from concurrent chart review) showed a significant association between total dex exposure and cataract severity (coefficient estimate [ce] 0.255, p< 0.05), which was confirmed by correlation analysis (r=0.143). However, age at cataract onset (ce 0.004, p=0.81) and dex dose per cycle (ce -0.004, p=0.19) did not show a significant relationship with cataract severity.
Conclusions: Of pts with MM who develop cataracts, almost half rate their cataracts as disruptive or severely disruptive to QOL. Over 30% of pts who report cataracts recall developing this toxicity within 6 months of exposure to dex-containing regimens, a concerning finding given that pts may remain on dex for years with regimens like Dara-Kd or Isa-Kd in the relapsed setting. While limited by recall bias and lack of a control group who did not develop cataracts, strengths of our analysis include its direct focus on the pt experience. Given the unclear contribution of dex to most MM regimens apart from preventing infusion reactions during the 1st cycle, discontinuation of chronic dex after the first few cycles should be considered in all pts with MM and not just for frail or late-line pts.
