Treatment of Relapsed/Refractory Myeloma
Poster Session 2
P-245: Belantamab mafodotin in patients with severely impaired renal function: a phase I, 2-part study to evaluate pharmacokinetics, safety and efficacy in patients with relapsed/refractory multiple myeloma
Thursday, September 28, 2023
12:30 PM - 1:30 PM EEST

Sosana Delimpasi, MD
Department of Hematology and Bone Marrow Transplantation Unit
General Hospital Evangelismos
ATHENS, Greece
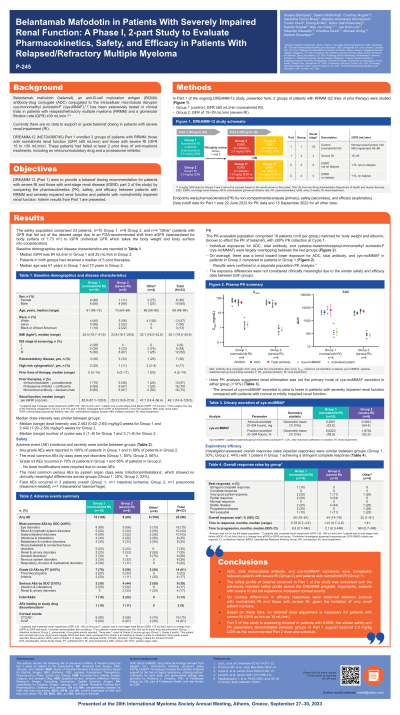
Introduction: The B-cell maturation antigen (BCMA)-targeting antibody-drug conjugate (ADC) belantamab mafodotin (belamaf) contains the cytotoxic molecule cysteine-monomethyl auristatin-F (cys-mcMMAF). Belamaf has been extensively tested in clinical trials at 2.5 mg/kg every 3 weeks (Q3W) in patients (pts) with relapsed/refractory multiple myeloma (RRMM) and a glomerular filtration rate (GFR) ≥30 mL/min. DREAMM-12 includes renally impaired pts (GFR < 30 mL/min) to provide belamaf dose recommendations for this population.
Methods: In Part 1 of the ongoing DREAMM-12 study (NCT04398745), 2 groups of pts with RRMM (≥2 lines of prior therapy) were studied: Control Group 1, GFR ≥60 mL/min (normal/mild renal impairment [RI]); Group 2, GFR of 15−29 mL/min (severe RI). Pts were treated with belamaf (2.5 mg/kg Q3W). Endpoints were pharmacokinetics (PK) by non-compartmental analysis (primary), safety (secondary) and efficacy (exploratory).
Results: Median (range) GFR was 84 mL/min (67–129) in Group 1 (10 pts) and 25 mL/min (20–28) in Group 2 (9 pts). Pts in both groups had received a median of 5 prior therapies. Median age was 61 years in Group 1 and 73 in Group 2. Median dose intensity was similar between groups. The PK population comprised 16 pts (n=8 per group) matched for body weight and albumin, with ≥80% PK collection at Cycle 1. PK analysis showed pts in Group 2 had lower geometric mean ADC plasma concentrations, total antibody and cys-mcMMAF than pts in Group 1. Exposures between groups were largely overlapping: differences were not considered clinically meaningful and were confirmed in a separate population PK analysis [1]. Urine PK analysis suggested renal elimination was not the primary route of cys-mcMMAF excretion (median < 10%). Adverse event (AE) incidence, severity and duration was similar between groups (any AE: Group 1, 100%; Group 2, 89%; Grade ≥3 AEs, Group 1, 70%; Group 2, 56%). There were 3 fatal AEs (Group 1, n=1, intestinal ischaemia; Group 2, n=2, pneumonia, intracerebral haemorrhage). The most common AEs by class (eye disorders: Group 1, 80%; Group 2, 56%), and most common serious AE (infections/infestations: Group 1, 20%; Group 2, 22%) showed no clinically meaningful differences across groups. Investigator assessed overall response rates (≥partial response) were n=5 of 10 pts in Group 1 vs n=4 of 9 pts in Group 2.
Conclusions: No clinically meaningful PK, safety or efficacy differences were seen between pts with normal/mild RI (Group 1) and severe RI (Group 2): based on these data, no belamaf dose adjustment is necessary for pts with severe RI and GFR as low as 15 mL/min. Part 2 of this study will assess belamaf 2.5 mg/kg Q3W in pts with end stage renal disease (GFR < 15 mL/min) on and not on dialysis.
Methods: In Part 1 of the ongoing DREAMM-12 study (NCT04398745), 2 groups of pts with RRMM (≥2 lines of prior therapy) were studied: Control Group 1, GFR ≥60 mL/min (normal/mild renal impairment [RI]); Group 2, GFR of 15−29 mL/min (severe RI). Pts were treated with belamaf (2.5 mg/kg Q3W). Endpoints were pharmacokinetics (PK) by non-compartmental analysis (primary), safety (secondary) and efficacy (exploratory).
Results: Median (range) GFR was 84 mL/min (67–129) in Group 1 (10 pts) and 25 mL/min (20–28) in Group 2 (9 pts). Pts in both groups had received a median of 5 prior therapies. Median age was 61 years in Group 1 and 73 in Group 2. Median dose intensity was similar between groups. The PK population comprised 16 pts (n=8 per group) matched for body weight and albumin, with ≥80% PK collection at Cycle 1. PK analysis showed pts in Group 2 had lower geometric mean ADC plasma concentrations, total antibody and cys-mcMMAF than pts in Group 1. Exposures between groups were largely overlapping: differences were not considered clinically meaningful and were confirmed in a separate population PK analysis [1]. Urine PK analysis suggested renal elimination was not the primary route of cys-mcMMAF excretion (median < 10%). Adverse event (AE) incidence, severity and duration was similar between groups (any AE: Group 1, 100%; Group 2, 89%; Grade ≥3 AEs, Group 1, 70%; Group 2, 56%). There were 3 fatal AEs (Group 1, n=1, intestinal ischaemia; Group 2, n=2, pneumonia, intracerebral haemorrhage). The most common AEs by class (eye disorders: Group 1, 80%; Group 2, 56%), and most common serious AE (infections/infestations: Group 1, 20%; Group 2, 22%) showed no clinically meaningful differences across groups. Investigator assessed overall response rates (≥partial response) were n=5 of 10 pts in Group 1 vs n=4 of 9 pts in Group 2.
Conclusions: No clinically meaningful PK, safety or efficacy differences were seen between pts with normal/mild RI (Group 1) and severe RI (Group 2): based on these data, no belamaf dose adjustment is necessary for pts with severe RI and GFR as low as 15 mL/min. Part 2 of this study will assess belamaf 2.5 mg/kg Q3W in pts with end stage renal disease (GFR < 15 mL/min) on and not on dialysis.
